Heartburn
Overview
Heartburn is a burning pain in your chest, just behind your breastbone. The pain is often worse after eating, in the evening, or when lying down or bending over.
Occasional heartburn is common and no cause for alarm. Most people can manage the discomfort of heartburn on their own with lifestyle changes and over-the-counter medications.
Heartburn that is more frequent or interferes with your daily routine may be a symptom of a more serious condition that requires medical care.
Symptoms
Symptoms of heartburn include:
- A burning pain in the chest that usually occurs after eating and may occur at night
- Pain that worsens when lying down or bending over
- Bitter or acidic taste in the mouth
When to see a doctor
Seek immediate help if you experience severe chest pain or pressure, especially when combined with other signs and symptoms such as pain in the arm or jaw or difficulty breathing. Chest pain may be a symptom of a heart attack.
Make an appointment with your doctor if:
- Heartburn occurs more than twice a week
- Symptoms persist despite use of over-the-counter medications
- You have difficulty swallowing
- You have persistent nausea or vomiting
- You have weight loss because of poor appetite or difficulty eating
Causes
Heartburn occurs when stomach acid backs up into the tube that carries food from your mouth to your stomach (esophagus).
Normally when you swallow, a band of muscle around the bottom of your esophagus (lower esophageal sphincter) relaxes to allow food and liquid to flow down into your stomach. Then the muscle tightens again.
If the lower esophageal sphincter relaxes abnormally or weakens, stomach acid can flow back up into your esophagus (acid reflux) and cause heartburn. The acid backup may be worse when you’re bent over or lying down.
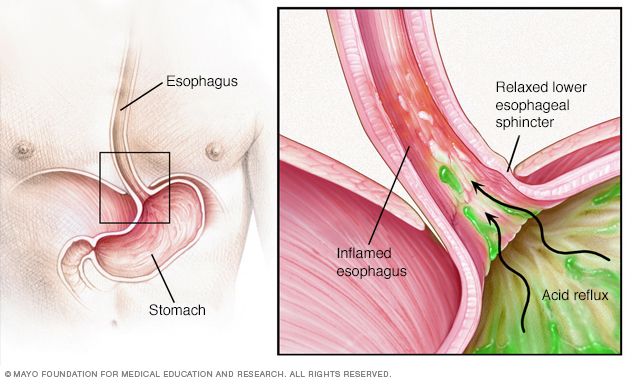
Acid reflux occurs when the sphincter muscle at the lower end of your esophagus relaxes at the wrong time, allowing stomach acid to back up into your esophagus. This can cause heartburn and other signs and symptoms. Frequent or constant reflux can lead to gastroesophageal reflux disease (GERD).
Risk factors
Certain foods and drinks can trigger heartburn in some people, including:
- Spicy foods
- Onions
- Citrus products
- Tomato products, such as ketchup
- Fatty or fried foods
- Peppermint
- Chocolate
- Alcohol, carbonated beverages, coffee or other caffeinated beverages
- Large or fatty meals
Being overweight or pregnant also can increase your risk of experiencing heartburn.
Complications
Heartburn that occurs frequently and interferes with your routine is considered gastroesophageal reflux disease (GERD). GERD treatment may require prescription medications and, occasionally, surgery or other procedures. GERD can seriously damage your esophagus or lead to precancerous changes in the esophagus called Barrett’s esophagus.
Diagnosis
To determine if your heartburn is a symptom of GERD, your doctor may recommend:
- X-ray, to view the shape and condition of your esophagus and stomach.
- Endoscopy, to check for abnormalities in your esophagus. A tissue sample (biopsy) may be taken for analysis.
- Ambulatory acid probe tests, to identify when, and for how long, stomach acid backs up into your esophagus. An acid monitor that is placed in your esophagus connects to a small computer that you wear around your waist or on a strap over your shoulder.
- Esophageal motility testing, to measure movement and pressure in your esophagus.
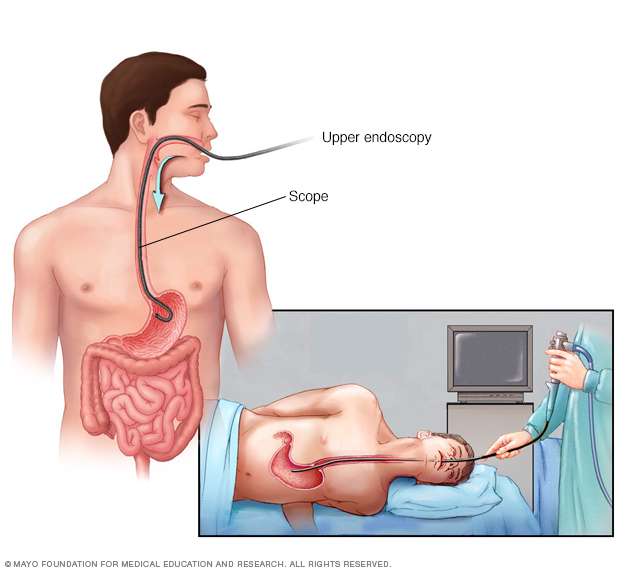
An endoscopy procedure involves inserting a long, flexible tube (endoscope) down your throat and into your esophagus. A tiny camera on the end of the endoscope lets your doctor examine your esophagus, stomach and the beginning of your small intestine (duodenum).
Treatment
Many over-the-counter medications can help relieve heartburn. The options include:
- Antacids, which help neutralize stomach acid. Antacids may provide quick relief. But they can’t heal an esophagus damaged by stomach acid.
- H-2-receptor antagonists (H2RAs), which can reduce stomach acid. H2RAs don’t act as quickly as antacids, but may provide longer relief.
- Proton pump inhibitors, such as lansoprazole (Prevacid 24HR) and omeprazole (Nexium 24HR, Prilosec OTC), which also can reduce stomach acid.
If over-the-counter treatments don’t work or you rely on them often, see your doctor. You may need prescription medication and further testing.
Lifestyle and home remedies
Lifestyle changes can help ease heartburn:
- Maintain a healthy weight. Excess pounds put pressure on your abdomen, pushing up your stomach and causing acid to back up into your esophagus.
- Avoid tightfitting clothing, which puts pressure on your abdomen and the lower esophageal sphincter.
- Avoid foods that trigger your heartburn.
- Avoid lying down after a meal. Wait at least three hours.
- Avoid late meals.
- Elevate the head of your bed if you regularly experience heartburn at night or while trying to sleep. If that’s not possible, insert a wedge between your mattress and box spring to elevate your body from the waist up. Raising your head with additional pillows usually isn’t effective.
- Avoid smoking and alcohol. Both smoking and drinking alcohol decrease the lower esophageal sphincter’s ability to function properly.
- Avoid large meals. Instead eat many small meals throughout the day.
Antacids
Usual Adult Dose for Dyspepsia
Chewable Tablets:
-Recommended dose: 1000 to 3531 mg orally up to 4 times a day as needed
-Maximum dose: 6750 to 7500 mg/day
-Duration of therapy: Up to 2 weeks